Background
PLATELETS & ATHEROTHROMBOSIS
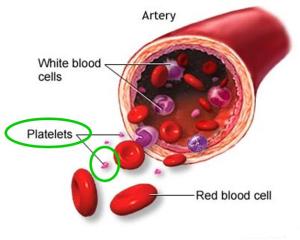
Platelets are the smallest of our blood cells. In fact, they are cell fragments derived from megakaryocytes in the bone marrow, and therefore lack a nucleus. They have a lifespan of about 7-10 days, and these cells are of outermost importance to us because they prevent blood loss. However, they are also involved in atherothrombosis, which is a cardiovascular disease. Circulating platelets will respond to a ruptured atherosclerotic plaque in the same way as if they encountered damage in the vessel wall. This means that they will become activated and trigger the formation of a hemostatic plug (an aggregate). In the case of a vascular damage, this plug would protect us from blood loss. However, in the case of a ruptured plaque, the plug would be formed inside the vessel and thus block the blood flow. A decreased blood flow leads to hypoxia (low levels of oxygen) in the surrounding tissues, possibly resulting in tissue death. If the plug is formed in vessel supplying the heart, a heart attack may arise.
PAR1 & PAR4
The drugs currently used in the treatment of thrombosis result in unwanted side effects, such as excessive bleeding. Therefore, it is important to find new targets for the creation of new, better drugs. Two such potential targets are platelet protease activated receptors (PARs) responding to thrombin: PAR1 and PAR4.
Thrombin, which is a protein circulating in our blood, is the most effective platelet activator. PAR1 and PAR4 are G-protein coupled receptors (GPCRs) with different affinities for thrombin. PAR1 is a high affinity receptor, meaning that it responds to low doses of thrombin, while PAR4 is a low affinity receptor, that thus responds to high(er) doses of thrombin. These receptors, as mentioned above, may be important therapeutic targets for the future treatment of thrombosis.
When receptors are possible new targets in medicine, it is always important to clarify their properties and signaling pathways, in order to elucidate all the possible effects of inhibiting the receptor. In this case, either of the PARs may be suitable targets. If we could find differences between the receptors, it would be possible to target only one of them without affecting the other (which is usually preferable).
THIS STUDY
In our study, we focused on two aspects that might differ between the receptors. The first subject was the platelet inhibitor nitric oxide (NO). Endothelial derived NO induces vasodilation (relaxation of the vessel) and inhibits platelet activation/aggregation. Thrombosis is characterized by a decreased release of NO, which means that these patients have an increased risk of platelet aggregation and plug formation inside the blood vessels. Investigating whether this antiplatelet mediator differently affects PAR1 and PAR4 was therefore of great interest.
The second aspect of our study was to clarify whether the receptors have different abilities to undergo desensitization*. The activation of PAR1 or PAR4 by thrombin is irreversible, because it exposes their tethered ligands which are then always available to interact with their receptor. To avoid prolonged signaling, there are mechanisms to shut it off. One of these is receptor desensitization, which is a common feature of GPCRs. Therefore, we wanted to see whether PAR1 and PAR4 have different abilities to undergo desensitization.
*when the receptor no longer responds to stimulation
AIM:
- Clarify differences between PAR1 and PAR4
HYPOTHESES:
- NO (a platelet inhibitor) differently affects PAR1- and PAR4-mediated platelet activation
- PAR1 and PAR4 differ in their ability to undergo desensitization
Responsible for this page:
Director of undergraduate studies Biology
Last updated:
05/18/09